Earlier this summer, our founder, Julie Evason, took part in an impressive, thought-provoking and highly insightful panel hosted by the Professional Record Standards Body (PRSB) entitled ‘Ill Health to Prevention’. It was recorded, and can be viewed via YouTube. The discussion brought together highly respected voices in public health to explore how data, leadership and lived experience can transform prevention from a peripheral ambition to a central tenet of healthcare delivery. Julie joined:
🔹 Sarah Arnold, Senior Policy Lead at The King’s Fund
🔹 William Roberts, CEO of the Royal Society for Public Health
🔹 Dr Abraham George, Assistant Director and Consultant in Public Health at Kent County Council
Together, they explored one of the most urgent questions facing the NHS: How do we move from reactive treatment to proactive prevention, using digital tools and community insights to improve population health?
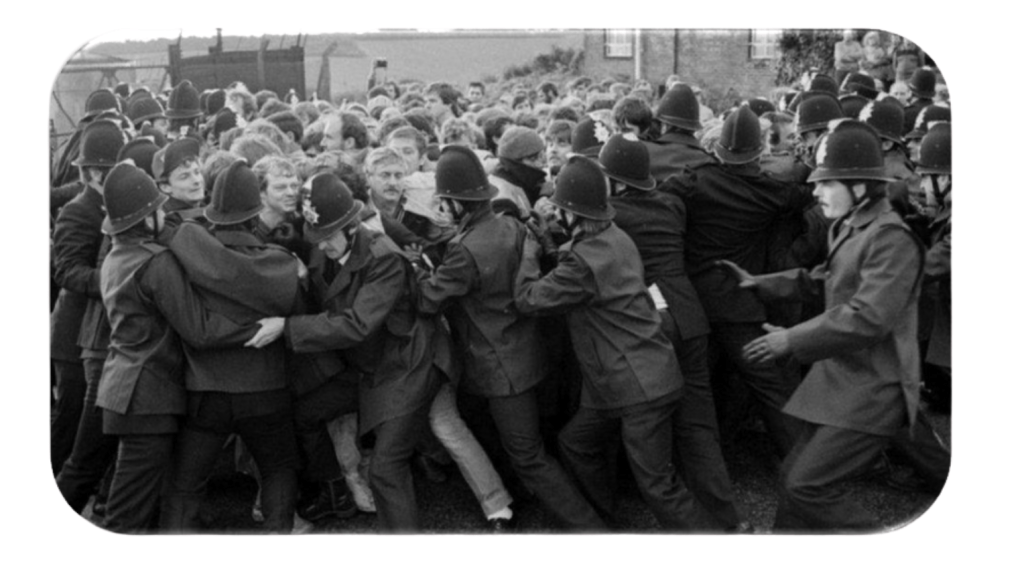
40 years working in Prevention
Julie’s contribution is rooted in decades of experience at the coalface of preventative health — quite literally. As she mentioned In her introduction, “Back in 1984, the police clashes with miners during the strikes highlighted a real lack of fitness across the police forces. It shone a light on the importance of being fit to do a job… The potential to improve fitness generally was becoming apparent.” (Julie co-founded Fitech: Fitness Through Technology in the 80s, which supported fitness across the police and fire services, many years before setting up Health Diagnostics.) Since NHS Health Checks launched in 2009, we’ve partnered with 70+ local authorities to deliver preventative care.
Prevention: What’s Blocking Progress?
This excellent panel tackled some of the structural and cultural challenges facing prevention in the NHS today. Sarah Arnold from The King’s Fund made the point that previous governments have proffered much rhetoric about health prevention, but have delivered less in terms of action. She drew attention to 6 gaps revealed by interview-based research into opportunities and barriers to CVD prevention, nationally and locally. These included:
- What ‘prevention’ means – “If you talk to people within the NHS, they generally seem to view secondary prevention as activity ‘in the NHS’… Whereas primary prevention is basically anything done ‘outside the NHS’. That might seem like an academic or semantic difference, but I think it’s a problem because it often feels like people are talking at cross purposes. And that can mean activity isn’t coordinated or optimal from a cost-effective population health perspective. And there may be gaps in activity.” Sarah noted a lack of alignment on the Goals of Prevention, “Is it about reducing demand on services, early mortality or improving health life expectancy? Different interventions are more effective at different outcomes…. We heard that the goalposts shifted quite regularly, making it difficult to plan.”
- Accountability – “Who’s responsible, and how are they held to account? This is of particular concern, given all the reshaping happening.”
- Funding – “Prevention hasn’t had the same injection of cash or promise [as shifts from hospital to-community, and to digital]….Many interventions are reliant on small, non-repeated funding pots which systems have to bid for – often at short notice, and in competition with each other”
- Effective Use of Digital Tools – Many ICBs and GPs weren’t making the best use of existing available data and tools. There are some really good tools… but they weren’t being taken up very widely. Every time I’ve heard Wes Streeting speak recently, he’s repeated the phrase, ‘The NHS has more pilots than British Airways.’ The focus should be on how to make them [the tools] spread.
- Skills and Leadership – “It’s not just about providing tools. Staff need the skills and capabilities and confidence to use those tools. Local areas in particular need the operational management capacity to support with the nuts and bolts of implementation…And the analytic expertise to work with data.”
- Integration and working in partnership – “You can have all the data in the world and identify things, but there’s need for integration, and to work in partnership…. You can have the greatest impact at population level if you focus resources at high-risk communities… But you also need to engage with people – send links to voluntary and community sector organisations to reach out effectively. And work with place-based partnerships and local communities to understand local needs.”
Sarah finished by adding, “The number one thing that needs to happen to make a real difference is to have a strong vision and mission for what prevention is for. And what was in The 10 Year Plan was this: ‘In ten years’ time, we will have transformed the nation’s health, restarted progress on longevity and healthy life expectancy, and begun narrowing the wide and widening health inequalities that unjustly divide our country.’ That to me is not very strong… It’s only in ten years time? There needs to be much most strong ambition, and I hope to see that in implementation plans and wider plans going forward with a focus on prevention.
Lessons from the Frontline
Julie shared her real-world reflections on what works, and the other experts agreed with many, including how a ‘brand’ can build trust – as with Measure Your Pressure and Check4Life. In addition, she showed the following work well:
- High-quality, real-time data for proactive management of programmes
- Strong leadership and a clear vision
- Patient focused consultations to clearly convey the impact that small changes can make on health and wellbeing, and what support is available
Community delivery — in accessible venues at convenient times (e.g. pharmacies, workplaces, mosques, temples, shopping centres). - Return of data to the patient’s record
These elements build trust, improve outcomes and offer measurable return on investment. Echoing Sarah, Julie noted that inconsistent funding, data access and national variations remain major hurdles.
Data Alone Isn’t Enough
On the subject of the need for high quality data, William Roberts of the RSPH explained how having it enables us all to do 4 things:
- Understand populations – what’s happening for people
- Think about their problems
- Understand what impact you might have, which solutions may work
- Understand the outcomes you have.
He sounded an optimistic note about the future of health prevention, reflecting that, “We’ve been trying to do this stuff for a hundred years, and we have had real success. I think one of the challenges is… When you get these big plans coming out, people see them as binary – ‘success or failure’… If anybody wants to talk about the greatest hits, and what we’ve done in terms of prevention over the last 200 years, I can bore you for England! This is stuff that’s happened within very short spaces of time in prevention.”
Noting the need for strong leadership, William explained that at some point, you need to be confident enough to take a gamble on the thing you need to go after. For him this means asking, “Where do you get the biggest gains in a system? For example, if you look at [NHS] Health Checks, they’re amazing. The single greatest benefit we could have is going back to the people who’ve already been diagnosed with high blood pressure in health checks. Three million of them aren’t on treatment. We know who those people are. We could do something for them tomorrow. The question therefore is, why don’t we go after them, instead of just going after new people to do more testing, but not necessarily converting them into treatment.”
Interestingly, William added a factor our team observes each and every day: “It’s people who make plans happen. Plans don’t.” So while data is vital — helping us understand populations and measure outcomes — the challenge lies in knowing when to act. In his words, “Aortic aneurism screening is a really good example of that. We know who’s most likely to have it. We know where they’re most likely to be, and we could go after those populations.”
Making Tech and Data Work Locally
Dr Abraham George echoed the need for better infrastructure and leadership at the local level by having:
- Integrated digital systems to share clinical and socioeconomic data
- Robust governance, especially across complex landscapes like Kent
- A ‘data economy’ mindset, where sharing is standard and secure
- Local leaders empowered to make decisions without waiting for top-down directives
His tone was pragmatic: “We could have made more progress. The NIHR is focusing more on prevention now, and we are seeing positive shifts in social care. But we need to do more.”
A Call to Action
Finally, Julie emphasised the practical changes needed to embed prevention into the fabric of the NHS, urging the sector to:
- Stop reinventing the wheel — proven models exist
- Standardise and improve data quality
- Target the right populations using patient data
- Ensure interoperability with clinical systems
- Use technology as a facilitator, not a barrier
- Make tech accessible and meaningful to users
- Establish follow-up support via local hubs
- Measure long-term outcomes to secure lasting investment
On the subject of being meaningful, she added, “It’s not just about building better systems — it’s about giving people a reason to engage and improving future health.
Looking Ahead
In summary, as the panel made clear, prevention is no longer ‘optional’: With rising health inequalities, workforce challenges and mounting costs, it must be a central pillar of our health and care system. At Health Diagnostics, we remain committed to turning insights into impact. As William Roberts said, “Change happens at the speed of trust.” That trust starts with people, data, and the ambition to act — not just to plan.
