
Since 2009, the NHS Health Check has played a crucial role in preventative healthcare in England, targeting major health risks such as heart disease, stroke, diabetes, and kidney disease. Designed for individuals aged 40-74 without pre-existing cardiovascular conditions, the Programme aims to detect health issues early, and facilitate timely interventions. The rationale in doing so is to address the enormous burden of ill-health caused by cardiovascular disease (CVD): a condition which the National Audit Office points out, “contributed to a quarter of deaths in England” in 2022.
Despite increasing evidence underscoring its benefits, the Programme has faced persistent scrutiny, often rooted in outdated studies or misinterpretations of data. This blog reviews the evolving evidence base behind NHS Health Checks, beginning with earlier studies that established its foundational impact, followed by a closer look at the latest research findings. Of particular importance is a groundbreaking 2024 study which suggests the Programme is associated with highly significant health benefits. Finally, we examine the economic case for NHS Health Checks, discuss challenges in their delivery, and outline pathways to further improve uptake and effectiveness.
Reviewing the Early Evidence
The NHS Health Check Programme has been subject to multiple evaluations over the years. A comprehensive review of the evidence to date – the BMJ Rapid Review Update (2022) – extended the findings from a similar review conducted in 2017. (For more detail, see the NHS Health Check website). This 2022 update reinforced the Programme’s ability to identify cardiovascular risk factors and conditions, with the authors writing that:
“NHS Health Checks led to an overall increase in the detection of raised risk factors and morbidities including diabetes mellitus, hypertension, raised blood pressure, cholesterol and chronic kidney disease”
Additionally, offering NHS Health Checks opportunistically was noted to increase attendance among men, younger individuals and those with higher levels of deprivation; i.e. some of the key groups at heightened risk of cardiovascular disease (CVD). However, the authors also noted disparities in uptake across different population groups, suggesting the need for more targeted engagement.
Despite these positive findings, scepticism has remained. A significant factor shaping public and professional attitudes was an early Cochrane Review which cast doubt on the efficacy of general health checks. What hasn’t been so well-reported is how dated the vast majority of studies included that Review were. Indeed, Celeste McCracken, lead author of an influential 2024 study of these studies notes that:
“Two-thirds of the RCTs included took place in the 1960s-1970s, with the most recent reported from 1999.”
As a result, the insights derived from the Cochrane Review do not reflect the current structure and delivery of NHS Health Checks. Unlike any of the initiatives included in the Cochrane Review, the NHS Health Check Programme dates from 2009, and brought together a range of key individual risk factors for CVD. Strong evidence supports addressing these risk factors, which is why they are included in a thorough consultation process.
Furthermore, in our experience of working with countless stakeholders over a decade and a half, the influence of the Cochrane Review may have created a ‘self-fulfilling prophecy’: when expectations for impact are low, implementation may lack the necessary vigour, leading to suboptimal outcomes. We believe this can work both ways. For example, recent data from well-executed NHS Health Check initiatives, such as those in Medway Council (detailed below), show that when delivered effectively, and with energy, the benefits can be substantial.
New Evidence: The 2024 Study
A landmark study published in BMC Medicine in early 2024 assessed the medical records of 48,602 people who underwent an NHS Health Check (or its Scottish equivalent, Keep Well) compared with a matched group who did not. The results were striking:
- A 23% reduction in mortality among those who attended the check.
- Lower risk of dementia, heart attack, and death over an average 9-year follow-up.
- Higher diagnoses of diabetes, high cholesterol, and hypertension in the first 2 years following a check, allowing for earlier intervention and treatment.
- Greater engagement between clinicians and patients, leading to more effective long-term health monitoring.
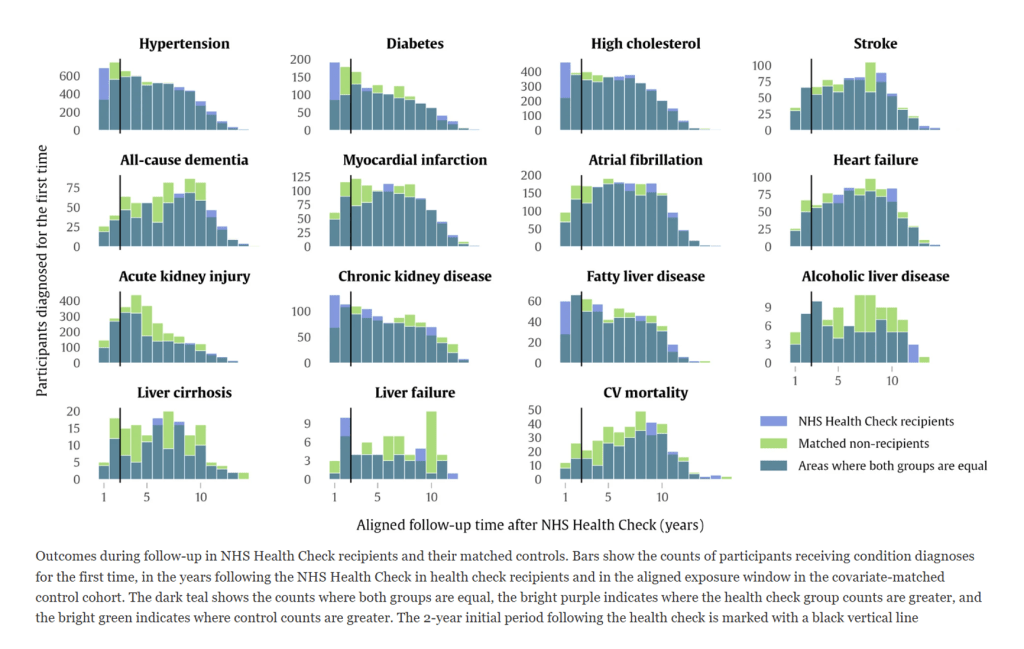
The figure below is replicated from McCracken et al (2024) (see Fig.4). Using data visualisation, it details some key findings from this research:
These findings provide a compelling counterpoint to past scepticism. Yet, despite this, certain figures such as Tom Marshall, Professor of Public Health and Primary Care at the University of Birmingham, have argued that the mortality reduction figure is implausibly high. In his words:
“The study suggests a 23% reduction in mortality with a Health Check. This is greater than the effect of treatment with a statin (8% reduction) or with an antihypertensive treatment in people with high blood pressure (13% reduction) or both treatments combined (20% reduction)”
As Marshall’s comment exemplifies, pharmaceutical interventions – rather than lifestyle change – are often the main, if not the sole, focus of attention amongst some stakeholders. In our view, this goes to the heart of what needs to change: too many people do not recognise or acknowledge the tremendous benefits that can be realised from meaningful lifestyle change. Indeed, this is something that is entirely ignored in Marshall’s calculations cited above.
While lifestyle change may be much more challenging to measure and research, compared to administering medication, it is nonetheless crucial that the research community does so. Crucially, McCracken et al (2024) in this latest study used large-scale, real-world UK Biobank data captured over a period of 9 years to assess what actually occurred within the population. Given the stated emphasis of the NHS Health Check, and its capacity to create ‘teachable moments’ and inspire lifestyle improvement, the hypothesis would be that behaviour change may be an important factor in some of the impressive results identified. As McCracken herself observes in response to Marshall’s critique:
“There are many things we simply cannot know about how people engage with our NHS (and what happens afterwards) without looking at their real-life health records […] There is not a great difference between the 23% reduction in mortality risk that we found, and the 20% reduction quoted. The NHS Health Check serves as an early access point to multiple pharmacological, behavioural, diagnostic, and interventional pathways as outlined in NICE guidelines, which GPs routinely use for onward referrals.”
Further Supporting Evidence
The key point we want to stress is that earlier detection through NHS Health Checks can facilitate a broader range of interventions which include – but are by no means exclusive to – medicalisation. Additional key studies have reinforced the positive impact of NHS Health Checks in this respect. These include:
- BMJ Rapid Review Update (2022): Found increased detection of cardiovascular risk factors and conditions, although uptake varied across population groups.
- BMJ Multimorbidity Study (2020): Strengthened the case for prevention, demonstrating the long-term benefits of early intervention.
- BMJ GENVASC Study (2023): Showed that the majority of patients identified with high CVD risk through the programme received effective clinical interventions – although a third did not receive follow-up care, highlighting an area for improvement.
- BJGP Comorbidity and Management Study (2017): Found that statin prescriptions were 40% more likely among NHS Health Check attendees than non-attendees, leading to significant public health benefits.
Room for Improvement
Several studies highlight both the barriers and opportunities to improving NHS Health Check delivery. For example, an analysis by Staffordshire University and commissioned by Public Health England (2021) on physical activity and alcohol measurements in NHS Health Checks found that key assessment tools were often underutilised, pointing to gaps in service delivery, and the need for more comprehensive discussions with patients.
One solution to this gap lies in better integration of digital tools to support clinicians and ensure both quality and consistency in NHS Health Check delivery. Our Interactive Consultations system addresses this challenge by providing clear prompts to help providers communicate what an individual’s risk means for them. Effective communication is essential, if the contact is to function as a gateway to behaviour change. .
In addition, the in-built quality-assurance mechanisms within Interactive Consultations such as automated reminders also prevents incomplete checks. This is a persistent problem which can undermine the quality of delivery. The impact of this fail-safe approach is evident in our work with Merton Health: before implementing our system in 2021-2022, significant numbers of checks were being marked as incomplete, which necessitated costly and time-inefficient follow-ups to ensure patients received a full review. Now, with our system in place, completion rates have reached 100%.
The importance of digital integration is further reinforced by a 2021 NHS Health Check delivery model survey which found that adopting digital tools could help standardise quality, improve consistency and expand the Programme’s reach. Based on our long-standing work supporting the NHS Health Check, these insights chime with our experience on-the-ground. By reducing variation in service delivery, technology-driven solutions have a pivotal role to play in making NHS Health Checks more effective and accessible to a wider population, especially those most in need.
The Economic Case
Beyond their health benefits, NHS Health Checks provide substantial economic returns. A recent National Audit Office (NAO) report entitled ‘Progress in preventing cardiovascular disease’ highlights the fact CVD is a major avoidable cause of death, costing billions to the economy. Given these vast costs, NHS Health Checks have significant potential to deliver value for money. Indeed, health economic modelling published by the Department of Health and Social Care indicates that for every £1 spent, the programme delivers a £2.93 return on investment – through improved health outcomes, reduced demand on healthcare services, lower social care costs and increased productivity.
However, a key challenge remains, namely, inconsistent commissioning of Health Checks across local authorities. The NAO has pointed out that despite the fact NHS Health Checks are a statutory responsibility, there is no effective system for their commissioning, leading to inefficiencies and regional disparities in delivery. At Health Diagnostics, we agree, and we advocate for a more streamlined, standardised national approach that could enhance uptake and ensure best practices are implemented consistently. For our full response to the NAO’s findings, see our blog.
Increasing Engagement and Optimising Delivery
Currently, only 46% of people who are invited to an NHS Health Check do attend it. Given the benefits detailed above, increasing participation is crucial. In our experience, the effectiveness of local programmes depends heavily on the quality of engagement from public health leadership and alignment among local stakeholders. Our impression, having supported the delivery of the Programme for over 15 years, is that when stakeholders are fragmented, inertia can set in, leading to fewer high-quality health checks, undermining faith in the Programme to support the kind of transformational change that it has the potential to deliver.
To address this, it is crucial that NHS Health Checks are not viewed as a ‘tick-box exercise’ but as an opportunity to engage individuals, helping them understand their results and the benefits of making lifestyle changes. Personalised risk communication (e.g. using tailored risk scores, or relatable analogies) has been proven to increase the likelihood of informed decision-making and promotes healthier behaviour change, especially when compared to generic materials. For instance, by explaining what a 10-year risk score might mean in terms of being able to stay active with grandchildren, or continue working. Studies show that framing health in relatable, story-based terms significantly improves recall – and motivation to change. Doing so effectively helps people stay healthier for longer, as evidenced by the latest research.
The NAO report also concludes that there is ‘no systematic targeting of those most at risk’, limiting the programme’s potential impact. Having recognised that this was an issue a number of years ago, we developed data-driven technology to mitigate it: Our technology has been created to be fundamentally geared towards empowering providers to stratify and segment their populations according to local priorities. We know that by leveraging innovative outreach methods and personalised engagement strategies, the reach and effectiveness of the programme can be significantly enhanced. (Our case studies, such as our work with Medway Council, speak directly to this.)
Proven Impact: Community-based Outreach
A 2025 study entitled “Barriers and Facilitators of NHS Health Checks in Socioeconomically Deprived Communities in the North East of England“ by Teesside University highlights key challenges, such as limited awareness, cultural perceptions of self-reliance and mistrust of healthcare systems – factors which can function together to prevent greater uptake. This study calls for culturally tailored communication and accessible, community-focused NHS Health Checks to engage underserved populations.
Health Diagnostics has been instrumental in demonstrating the effectiveness of community-based outreach providers. Research conducted in collaboration with Imperial College London, and published in BMC Health Services Research, conclude that community providers using our system:
“Effectively reach under-served groups by delivering preventive CVD services to younger, more deprived populations, and a representative proportion of ethnic minority groups.”
This finding is echoed by our work with Medway Council, mentioned above; an area which has partnered with us since 2020 to deliver the checks via GP practices, innovative community outreach and digital channels in an attempt to address local health inequalities, budget constraints and inefficient workflows. Based on the findings of an observational statistical analysis of the project, the significantly larger reductions in CVD risk scores (when baseline results were compared with follow-up within 12 months) were exhibited amongst individuals who were engaged-with by community teams using our system. Specifically, Medway’s community outreach approach led to a 10.5% reduction in CVD risk scores within a year (p<0.0001), compared to just 0.002% in a matched GP-based cohort (p=0.2526). This highlights the effectiveness of community outreach teams using Health Diagnostics’ system to drive meaningful health improvements
Conclusion
The latest research confirms that NHS Health Checks remain a vital component of preventative healthcare. While early evidence laid the groundwork for the Programme’s benefits, new studies decisively counter scepticism and demonstrate significant reductions in mortality and major health risks. Beyond health improvements, the economic case for NHS Health Checks is stronger than ever, especially given the current financial pressures on the NHS.
To maximise the full potential of NHS Health Checks, the focus must now be on expanding participation, optimising delivery models and enhancing community engagement. With the right approach – including integration of digital tools, and data-driven, innovative community outreach methods, NHS Health Checks can evolve into an even more powerful preventative tool – helping individuals live longer, healthier lives while also reducing strain on healthcare resources.
