Setting the scene
Despite challenging conditions and unprecedented demand, every day across the UK, NHS staff work tirelessly to improve peoples’ health and wellbeing. However, with so much energy channelled into providing world-class care to patients, the health of the health service itself can sometimes fall out of focus. In recognition of this situation, NHS England and Public Health England have, in recent years, placed an increasing emphasis on pioneering a “radical upgrade in prevention” for Britain’s most revered institution and its workforce. This emphasis was given renewed focus in January 2019 with the publication of the NHS Long Term Plan. Commenting on the release of the Plan, Simon Stevens – NHS England’s Chief Executive – publicly stated that the NHS has “got to do a better job of looking after the staff that we have. I think people are under huge stress and pressure”. It is this drive to support the health of NHS staff – and a specific example of an initiative in the South of England – that this article is concerned with.
Amongst the NHS trusts where new occupational health and wellbeing programmes have been rolled-out is East Sussex Healthcare NHS Trust (ESHT). With a staff population of over seven thousand people, ESHT is a large trust with a commitment to reducing sickness absence. In partnership with East Sussex County Council (ESCC) Public Health and Health Diagnostics, ESHT were one of several trusts to roll out a comprehensive NHS Health Check programme for eligible NHS staff. Funding came from ESCC Public Health, where it was recognised that the project was closely aligned with the objectives of the NHS Five Year Forward View and that it carried the potential to boost local NHS Health Check uptake. Health Diagnostics provided digital support and training.
Despite posing challenges, the service proved to be both popular and effective, with over one thousand staff receiving one-on-one support to address their cardiovascular risk. Following the programme, 64% of surveyed staff referred had undertaken lifestyle change (with a further 15% actively intending to make such a change). In the words of Kim Boorman – ESHT’s Staff Wellbeing Lead – outcomes such as these meant that the health checks proved to be “a really exciting and worthwhile project which engaged a significant number of the workforce”.
IT set-up and training
To ensure a patient-focused and fully IG compliant IT system was in place, ESHT and East Sussex County Council (ESCC) Public Health sought Health Diagnostics’ support. According to Kim, Health Diagnostics’ software “worked brilliantly and really guided the health check process, which was great for us because we had wellbeing advisers, as opposed to trained nurses, carrying out the appointments”. In addition to the consultation support tool, the software linked with local GP practices, thereby ensuring that eligible NHS Health Check results were transferred back to patients’ records.
An important factor in the successful set-up of the programme was the close collaborative working relationship that ESHT established with the local NHS Health Check commissioner, East Sussex County Council’s Health Improvement Principal, Hayley Martin. Through her support and liaison, Hayley helped ensure the ESHT NHS Health Checks aligned with the East Sussex NHS Health Check pathway. In addition, her involvement included working with ESHT and Health Diagnostics to forge links with local general practices and lifestyle service providers. Crucially, this allowed for data communication channels to be opened up between ESHT’s occupational health team and the local primary care network. Not only did this mean that the system was able to automatically and electronically send patients’ results securely to GPs, it also ensured that the NHS Health Checks completed at the Trust could be efficiently reported to ESCC, who report East Sussex NHS Health Check activity to Public Health England quarterly.
“Whilst Health Diagnostics were very supportive”, explains Kim, “one of the key lessons we learnt insofar as IT is concerned was that, when dealing with internal NHS IT departments, things can take longer than expected”. This led to one of the key learnings that Kim has highlighted for other NHS trust’s looking to introduce similar programmes:
LEARNING OPPORTUNITY 1: Engage with your trust’s internal IT as early as possible. If you need to get permissions from your trust’s IT department to install new software on the local NHS network, experience suggests that you may encounter delays.
In addition to the IT set-up, the Occupational Health Team brought on board two wellbeing advisors to carry out the health checks. To help establish the required competencies amongst this team, Health Diagnostics held a CPD-certified NHS Health Check training day that was fully aligned with Public Health England’s 10-step competence framework. As a result, the staff effectively acquired the necessary skills and knowledge; post-training knowledge checks came in at an average score of 82% (a significant increase of 24% on the pre-training scores), indicating the ability of delegates to deliver to the standards required.
Programme roll-out and staff recruitment
Kim and her team used a variety of methods to attract eligible staff to sign up for a check. From handing out flyers to putting up posters, a range of initiatives were employed to spread the message. Key opportunities for learning emerged from this promotional phase, including the benefit of getting senior management on board in the first instance:
LEARNING OPPORTUNITY 2: Engage your CEO early on. ESHT’s CEO was amongst the first people to receive a health check, which led to him approving that the health checks could be offered to staff in work-time due to their value and potential.
With staff able to take time out of their schedule to get their health check, the Occupational Health Team set about circulating personalised invite letters to staff. Whilst this proved to be an important recruitment method, it was nonetheless the cause for further learnings:
LEARNING OPPORTUNITY 3: When sending out invite letters to NHS staff, consider doing so by department. ESHT distributed invites alphabetically, from A-Z, across the trust. However, if they were to start the project afresh, they would seek to improve uptake by concentrating on one department at a time. The feeling was that this could have further supported promotion by ‘word-of-mouth’, as well as helping to focus the team’s administrative efforts.
In addition to this promotion, Kim herself put in a personal effort to ensure the programme was widely known about amongst the workforce; “I went trekking the wards with a timetable signing people up”, says Kim, “and despite the fact that the DNA rate was slightly higher with these bookings, it was definitely worth it in the long-run”. To ensure that all staff were given a convenient opportunity to access the service, the team set up nineteen roadshow clinics at smaller, more disparate, trust sites and departments. According to Kim, “this really helped us increase our uptake. We also found that our staff sometimes had difficulty getting the time away from the wards or their desk; the ‘mobile-approach’ meant that many more people were able to attend as they weren’t having to travel for their appointment”.
The NHS Health Check appointment
Despite the average NHS Health Check generally lasting between twenty and thirty minutes, Kim felt that the consultation presented a unique opportunity for staff to focus on their health and wellbeing and that “it would be best to really make the most out of that contact time”. As a result, it was decided that, for each appointment, forty minutes would be allocated.
Health Diagnostics’ interactive software was used during the appointments to guide the operators and staff through a range of tests and questionnaires. Each health check eventually culminated in a cardiovascular risk score and heart age calculation. Having been created to be closely compatible with motivational interviewing techniques, the software is particularly effective encouraging people to reflect on their health status. What’s more, as the results indicate, the consultations proved conducive to opening a gateway to on-going behaviour change. For Kim, having this system and Health Diagnostics’ support in place provided “real reassurance” that the data being collected was both accurate and informative for staff and operators.
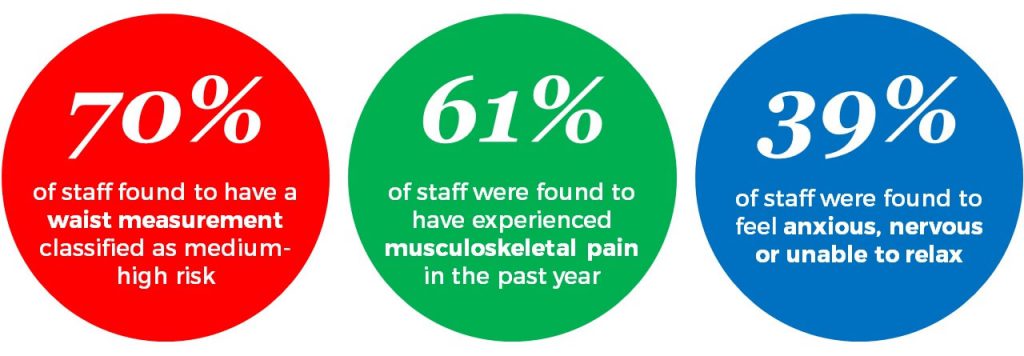
In addition to the standard tests that comprise the NHS Health Check, ESHT were also interested in assessing potential musculoskeletal disorders (MSK), and common mental health problems, such as depression and anxiety. Where relevant, early intervention and support was offered to help individuals reduce and manage the conditions. “A key reason for adding these components”, explains Kim, “is because MSK and mental health represent the two main causes of sickness absence at ESHT. We therefore needed to take the opportunity to address the issues, particularly as they can actually be quite closely linked”. According to the ONS, ESHT’s experience is not unique; nationally, MSK is the second and mental health is the third leading cause of sickness absence in England, after minor illnesses such as coughs and colds. In introducing these tests to the health check – as well as recognising their potential to be linked – ESHT have taken steps to locally fulfil the ambitions of the NHS Five Year Forward View, and dissolve “the classic divide […] between physical and mental health” .
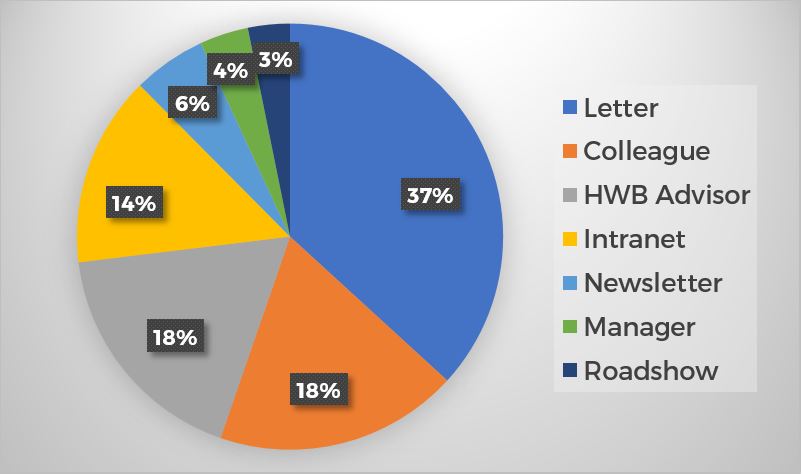
The reception of staff to the efforts of the team was overwhelmingly positive; 98% of respondents at the one-week follow up reported being satisfied-very satisfied with the experience of their health check. Something that was less pleasing to Kim and her team however was the number of people that were encouraged to attend by their line manager. As the pie chart below suggests, only 4% came via this route. It was felt that this may have impacted on the uptake and gave rise to another important learning opportunity.
LEARNING OPPORTUNITY 4: Ensure that line managers are engaged. Often, these are the people that need to release their staff to go for their health check, so it’s important that they’re on board and understand the value of the programme.
Results achieved and actions taken
Over 13 months, between February 2017 and March 2018, ESHT’s Occupational Health Team completed 1069 health checks – 82 each month – on staff across the Trust. With 3273 eligible individuals working at ESHT, this represented a 33% uptake and reflects the fact that Kim’s team made meaningful contact with 1/7 of ESHT’s workforce. Despite being slightly fewer than what the team had targeted themselves with, this uptake level was significantly higher than that seen within other NHS trusts running similar programmes (where the average uptake was 11%).
According to Kim, a variety of important outcomes came to light through the health check programme. Amongst the stand-out findings were the following:
Close links were also identified between elements assessed in the health check, with important insights established in relation to some of the areas highlighted above. For example, a link between feelings of anxiety and depression is abundantly clear in the data: the rate of staff that reported feeling depressed was over ten times as high in those that also experienced feeling anxious, by comparison to staff that didn’t feel anxious.
The known connection between mental ill health and MSK was also reflected in the outcomes: 25% more staff that experienced feeling anxious and depressed suffered with MSK pain, by comparison to those not reporting any mental health difficulties. For those concerned with being able to spot the signs and implications of ill health, these outcomes underline just how closely related issues affecting both mind and body may be.
With certain areas highlighted as local priorities for ESHT, the Trust has ensured that targeted interventions are in place to help support those at risk. The interventions, which align closely with the priority areas identified, include:
- Employment of a physiotherapist within the Occupational Health and Wellbeing Department to identify and treat cases of MSK and stress
- Provision of ‘stress-less’ courses, which have been over-subscribed
- Provision of workshops on resilience and wellbeing
- The introduction of a 12-week NHS healthy weight programme
- Development of healthy options in staff canteens and on-site cafes
In addition to the figures isolated in the data, Kim and her team repeatedly received positive personal feedback from staff, including reports of people dropping dress sizes and actively increasing the amount they exercise. Perhaps most significantly, numerous staff reported that being referred to their GP had resulted in high-risk conditions being identified and managed. Key examples of this include diagnoses of diabetes and high blood pressure. In the words of one such individual, “I was advised to go straight to my GP due to high blood pressure and now am on medication. I am so pleased and think the health check might have saved my life”.
Indeed, the number of GP referrals for high blood pressure was another noticeable outcome of the project; of the 371 referrals that were made to GP, 239 of these were due to suspected hypertension. Taking this parameter alone, if all the individuals referred to their GP for high blood pressure were to be effectively managed with anti-hypertensive treatment, research indicates that 7 cardiovascular events and 2 preventable deaths would be avoided amongst ESHT staff over 5 years .
Whilst management with medication is an important outcome of the NHS Health Check, inspiring lifestyle change is another. Despite it being harder to quantify the precise causal effects of lifestyle change, the potential benefit associated with embracing change – both personal and economic – is undoubtedly huge. Indeed, Harvard University recently calculated that adopting healthy habits could help women increase their life expectancy by 14 years, and men by 12. Such improvements to the health of NHS staff could function as a vital financial lifeline at a crucial time by helping to reduce the £2.4 billion that the NHS spends on sickness absence every year.
According to follow-up surveys returned from 38% of those that received a health check – 412 of the 1069 people tested – both lifestyle change and medical management have proven to be key outcomes of the workplace health check programme. The following data was recorded from individuals one month after they’d receiving the health check:
- 20% had been referred to their GP, with 60% of those referred following up with the GP within the month
- 14% had been referred on to lifestyle or occupational health services, with 30% of those referred attending within the month
- 64% of those referred on reported having made a lifestyle change within the month, with a further 15% reporting that they were intending to implement lifestyle change
Conclusions
Kim admits that, when the project began, she had been “quite sceptical about NHS Health Checks and wasn’t sure if the programme was a worthwhile use of resources”. Nonetheless, having seen its effects, ESHT’s Staff Wellbeing Lead confessed to having “completely changed” her mind. For the whole team, the programme proved to be a “really exciting and worthwhile” endeavour, which facilitated close engagement with a large proportion of the workforce and helped reveal life-saving information around undiagnosed conditions that certain staff were unknowingly living with.
Perhaps surprisingly, the programme was able to offer something new and valuable to experts in heart health. As Kim explains, “we had a number of cardiology doctors coming through and giving really good feedback. Whilst they obviously know a huge amount about the heart, the opportunity to have a chat and think about the possible impacts of their lifestyle was really useful for them”. As a result, further learnings emerge:
LEARNING OPPORTUNITY 5: Even for knowledgeable individuals that specialise in secondary care, there’s real value in being given a space to reflect and talk; the person-centred approach has a unique place when promoting health and wellbeing.
Having helped ESHT achieve its Health and Wellbeing CQUINS for 2017/2018 – and having been only one of three trusts in England to do so – the health check programme resulted in significant Trust-wide benefits. More importantly however, it had an overwhelmingly positive impact on the very people that uphold the health service across East Sussex: NHS staff at all levels. With the NHS continuing to experience unprecedented strain and demand, ESHT’s project represents an important template for how NHS staff can be individually supported to live healthier for longer.