Introduction
As many that are engaged with the NHS Health Check (NHSHC) will know, the Office for Health Improvement and Disparities (OHID) – the organisation that has taken over many of PHE’s functions – recently published their long-awaited review of the national programme. Wide-ranging in scope and sweeping in its implications, the review concludes with six key recommendations for the future of the NHSHC.
This article summarises those recommendations and outlines the ways in which Health Diagnostics are positioned to support health authorities deliver them. Despite the six recommendations being forward-looking, having worked on pioneering projects for over a decade, Health Diagnostics has prior experience of enabling each of them. Real-world examples are outlined in relation to each recommendation below.
Recommendation 1: Build sustained engagement
Recast the NHS Health Check around an ongoing relationship with individuals rather than delivering an isolated check. Ensure a clear focus on promoting lasting health and wellbeing, backed-up by effective communication of risk, support for behaviour change, and connections to other services that people need.
Supporting health check providers to make their contacts count has been at the heart of Health Diagnostics’ mission. Whilst historically, NHSHC projects in England have offered contact once every 5 years – and have therein, by design, reduced the chances of on-going contact – other health check projects have taken a different approach.
Aneurin Bevan University Health Board (ABUHB) – a health authority in South Wales named after the founder of the NHS – have, for years, done things differently regarding prevention and population health. A crucial way in which ABUHB’s approach has differed from that seen in England is in how multiple health checks have been offered to the residents of South Wales. This has allowed for ongoing relationships to be fostered, for health to be tracked in a longitudinal way and for lasting behaviour change to be supported.

A brief case study listing some of the outcomes seen on ABUHB’s ‘Living Well Living Longer’ programme is available online. Importantly, and unlike England’s NHSHC, if an individual’s CVD is equal to or greater than 10% and if the person has modifiable risk factors, ABUHB’s wellbeing advisors have been able to offer 6 months of intensive support. Provided via a mixture of phone calls and one-to-one meetings, all support has been aimed at empowering individuals to take control of their health.
Health Diagnostics worked closely with the ABUHB team to develop digital systems to enable the ‘review and monitoring’ functions required for this model. What’s more, the systems have techniques for encouraging behaviour change hard-wired into their design. From dynamic risk graphics to personalised advice, risk is communicated in ways that enable all individuals to get a clear understanding of what their health status means for them. Automated electronic transfers to local services also join-up and streamline referral pathways. Such joined-up working has enabled integration with, for example, local social prescribing services, as detailed here.
The outcomes from ABUHB’s programme speak for themselves. With significant improvements in blood pressure, reductions in cholesterol, and drops in risk-increasing lifestyle behaviours, ABUHB’s model has been successful at driving the very ambitions raised in OHID’s first recommendation. What’s more, the systems that have helped facilitate and capture these outcomes are proven and ready to deploy.
Recommendation 2: Launch a digital offer
Improve the accessibility and efficiency of the NHS Health Check via a digital offer. This will support a sustained relationship with the public. Retain a non-digital approach for those people who require or request it.
During the pandemic and with many NHSHC projects temporarily suspended, Health Diagnostics has been focused on pushing the envelope in terms of digital prevention systems. A key part of how we’ve achieved this is through the creation of a tool for enabling digital self-assessment. What this allows for is for multiple contacts to take place remotely and via digital means, as alluded to in OHID’s second recommendation.
Amongst the first to trial the self-assessment tool has been York & Scarborough Teaching Hospitals NHS Foundation Trust (Y&S). This award-winning NHS staff health check project has – much like the ABUHB project – been conducted without the restrictions of the NHSHC (i.e. Y&S use wider eligibility criteria than one check every 5 years and do not only offer them to people aged 40-74 without chronic conditions). Y&S have offered health checks to staff of all ages and, importantly, have also provided follow-up appointments for those wishing to improve their health. For a case study detailing the outcomes associated with Y&S’s programme, as well as details of how the team adapted during Covid-19, see this article.
The use of the digital self-assessment tool has meant that the Occupational Health Team at Y&S are now able to conduct health checks remotely. For any NHS staff that pass the set triage threshold, further in-person appointments can be arranged. On the other hand, those that are living healthily are provided with the tools and information to assist them to continue doing so. Feedback from users strongly suggests favourable experiences of engaging with their health in this way.
It’s technology of this kind that has seen Health Diagnostics, alongside Y&S, recently win the award for Best Wellbeing Initiative at Personnel Today’s Occupational Health and Wellbeing Awards, 2021. Furthermore, it’s also what’s seen Health Diagnostics shortlisted by PHE as one of a handful of organisations capable of delivering a fully digital NHS Health Check. In short, not only are Health Diagnostics able to support this key recommendation, we do so with technology that sits at the cutting-edge of the health tech sector.
Recommendation 3: Start younger
Make the NHS Health Check available to people from a younger age, when they are 30 to 39. Preventable risk factors such as smoking, high blood pressure, cholesterol and obesity drive the development of CVD and other diseases from early life.
As outlined above, Y&S’s project has involved offering health checks to all staff, regardless of age. A similar situation has been seen at Sheffield Teaching Hospitals NHS Foundation Trust (STH), where Health Diagnostics has supported the provision of another programme to provide health checks to NHS staff.
For the full story, STH’s case study can be accessed online. Crucially, the effects of widening the net of eligible individuals has contributed to profound improvements in a range of metrics. From the Trust’s perspective, reducing sickness absence across the staff cohort was a key objective. In the year following the staff health check programme’s introduction, STH saw:
- A 10% decrease in sickness absence compared with the previous year
- The fewest number of average working days lost compared with the previous 5 years
- The largest number of staff with no sickness absence compared with the previous 5 years
Outcomes such as these led to the Care Quality Commission (CQC) explicitly praising STH’s work and linking the improvements in staff sickness absence to the Trust’s new health and wellbeing policies. The outcomes also contributed to STH and Health Diagnostics being shortlisted in the Value-based Procurement category at the Academic Health Science Network’s (AHSN’s) NHS in the North: Excellence in Supply Awards, 2019.
From the perspective of targeting the NHSHC cohort (covered more in relation to recommendation 4), Health Diagnostics can assist local authorities and their providers to efficiently widen the pool of eligible individuals and target these people with an advanced range of predictive risk algorithms (e.g. to estimate those most at risk of CVD, diabetes, etc.). Importantly, these predictions can be done in both absolute and relative ways. This constitutes essential flexibility when engaging younger age groups; relative risk can be high in younger individuals – indicating potential health problems being stored up for the future – even if absolute risk (i.e. the risk of a CVD event over the next 10 years) is low.
Recommendation 4: Improve participation
Design and manage the NHS Health Check to improve participation by all eligible people, but especially the people likely to benefit most – those who live in more deprived areas, those from black and minority ethnic groups who are more susceptible to CVD, and men.
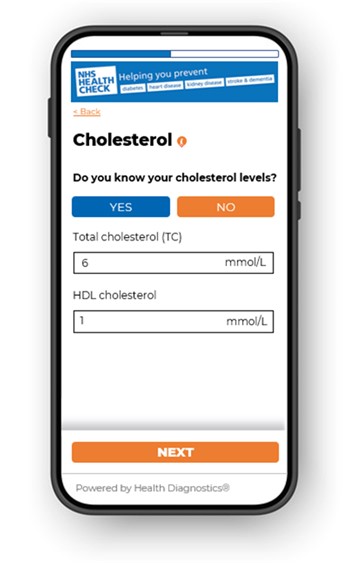
Helping to improve participation has always formed a focal point for Health Diagnostics. Economic modelling released in conjunction with OHID’s review emphasises why this is so important, with the return on investment (ROI) expected by 2040 steadily increasing from £2.93 per £1 spent (based on the current programme), to £3.27 per £1 spent if near total take-up is achieved.
Crucially, improving participation amongst the groups that stand to benefit most is where Health Diagnostics has placed a particular emphasis. According to research by Imperial College London, we – and the health authorities we support – have been able to facilitate precisely this. According to Woringer and colleagues, providers using Health Diagnostics’ IT solution “effectively reach under-served groups by delivering preventive CVD services to younger, more deprived populations, and a representative proportion of ethnic minority groups”, thereby working to “reduce health inequalities” and address the inverse care law,.
Providing the kind of targeting technology outlined at the end of the section above is, in part, how Health Diagnostics have supported these outcomes. What’s more, the targeted invites system we supply has led to areas seeing substantial increases in uptake, into the realms required to see the sort of ROI modelled by OHID. For instance, the graph depicts County Durham’s NHSHC uptake levels pre-, during, and post- Health Diagnostics’ involvement in supporting the invitation process. The area saw a 57% increase in uptake – up to 65% – through using the technology.
Recommendation 5: Address more conditions
As a first step towards a more holistic view of the health of the individual, consider the evidence on addressing the risk of common mental health and musculoskeletal conditions through the NHS Health Check.
Numerous projects that Health Diagnostics has supported have taken a broader view of health than the one suggested by the current mandated components of an NHSHC. Musculoskeletal (MSK) health, mental health and even cancer questions are amongst the additional conditions that we have supported providers to inquire about.
East Sussex Healthcare NHS Trust for instance specifically sought to understand the impacts of poor MSK and mental health on their staff. Interestingly, a relationship between these factors may be inferred, providing justification for the “more holistic view” OHID are advocating which sees the mind and body as intimately related. The following outcomes were observed:
- 61% of staff were found to have experienced MSK pain
- 25% more staff that experienced feeling anxious and depressed suffered with MSK pain, by comparison to those not reporting any mental health difficulties
- the rate of staff that reported feeling depressed was over 10 times as high in those that also experience feeling anxious, by comparison to staff that didn’t feel anxious
From a mental health perspective, Health Diagnostics has contributed to PHE’s Stakeholder Group tasked with working through the options and implications involved in incorporating mental health questions into the NHSHC. Having been included to advise on technological feasibility, Health Diagnostics – alongside Newcastle City Council and community providers in the North-East – have taken to piloting the scoped additions locally. The resulting findings, once published, stand to help inform practice-based evidence of how these recommendations can work on the ground.
Recommendation 6: Create a learning system
Launch a rigorous, ongoing independent scientific evaluation of the new NHS Health Check. The experience of delivering this service will offer a weight of data and learning, which should be evaluated in partnership with stakeholders. Collaborate with partners such as Our Future Health to test evidence-based innovations for future inclusion in the programme. This will create a ‘learning system’.
A culture of evaluation sits at the heart of everything that Health Diagnostics do. A long-standing relationship with the AHSN, award wins for research posters at PHE conferences, and collaborative research with Imperial College London’s Dept of Primary Care and Public Health that’s resulted in numerous published papers, all stand as testament to this commitment.
Health Diagnostics’ latest project with the Innovation Agency – the AHSN for the North-West Coast – and conducted in collaboration with Chester University, has involved a real-world validation study, conducted as part of the Health Matters Initiative. Whilst yet to publish findings, early indications are that the large project area examined which Health Diagnostics has been engaged with since 2017 may have helped contribute to significant drops in cardiac related A&E admissions and concurrent increases in statin prescriptions.
Such improvements are precisely what the LA Prevention Framework drives at. What’s more, they represent the sort of effects that contribute to the modelled ROI outlined in the response to recommendation 4. Whilst yet to be subject to peer-review, it is anticipated that the AHSN collaboration findings will be able to be announced early in 2022.
Glossary of acronyms
- ABUHB: Aneurin Bevan University Health Board
- AHSN: Academic Health Science Network
- CQC: Care Quality Commission
- CVD: Cardiovascular disease
- MSK: Musculoskeletal health
- NHSHC: NHS Health Check
- OHID: Office for Health Improvement and Disparities
- PHE: Public Health England
- ROI: Return on Investment
- STH: Sheffield Teaching Hospitals NHS Foundation Trust
- Y&S: York & Scarborough Teaching Hospitals NHS Foundation Trust